


Your life is regimented, predictable, and probably pretty simple (and possibly boring). You are now living in a nursing home amongst the familiar faces of other much older residents, and you feel you don’t fit in. Then without warning you feel strange and show signs of agitation, depression, or some new ailment. The doctor is called and a new medication is administered to counter the new symptom. You were meant to get better, but you react badly to the medication and have exaggerated behaviours and become agitated and start hitting out. You did not ask for a new tablet to try, you were made to take it and it makes you feel strange and behave in a different manner. Other residents are confused and startled by your unusual behaviour, they are rattled and start to yell at you. All of a sudden the whole place is in chaos …all because of you.
As a result an ambulance turns up with a person in a green jumpsuit (but you don’t see the ambulance). People are constantly talking at you, but it sounds like ‘white noise’ and they want you to be strapped into a bed like contraption. You refuse as you don’t know what is going on. People are scattering everywhere, fire doors are being locked and you are on one side of the clear doors and every other resident is on the other side. You start pulling at the doors trying to get to the familiar faces you can see through the window. You feel like a prisoner being put in isolation. You are now frightened and angry and have no idea what is going on – every move you make now has a consequence. The more you shake the doors the more people are yelling at you to calm down…you think to yourself “what is happening to me, I haven’t done anything wrong?”.
People are grabbing at you trying to settle you down, they tell you to go everywhere you don’t want to. The people send you to your bedroom. You think to yourself ? “I am not a child”…. but you are being constantly told to go. People stand in your way and block your exit, and you feel trapped. You are refusing to comply and along comes two more people in green suits. You are now cornered in your room and surrounded by 5 people telling you to calm down. Your mind is racing “How do I get out?”.
The green suits want to give you a needle but it is too dangerous. They opt for a nasal spray. Being blasted with spray up your nose is unpleasant, you need to be still and calm. You are told to lay down. You don’t want to, you sense something is bad about to happen. “HISSSSS” the spray is set off. You react really badly like a caged lion. Your mind is scrambled and you think again…. “Why are these people trying to hurt me?”. You are now in survival mode.
The green suit tries again to give you another spray, you hit her away. A heavy net blanket is thrown over you and you are pinned. They spray again, you struggle and are restrained. You thrash and bite as your arms and legs are pinned. You are placed in a strange tube like space and you are now moving. The ambulance races to the hospital and you start to calm down and are exhausted. You arrive at a very busy Emergency Department but you don’t understand this, there are stretcher beds with people on them all lined up. There are up to 10 green suits all walking around. Big muscle-bound men in navy uniforms are lurking nearby, you think to yourself “where am I?…What is going to happen next?..why are there so many people here?”. You are confused and lost, you are also angry and frustrated. The green suits are replaced by people in white outfits. Here comes another needle. You don’t want it…are they trying to drug you? ….Who are these people? You react by swiping at the person in white. You are then surrounded by 6 huge men. They are holding every limb down to the bed. An hour later you are still in the same position. More needles, More holding down, more fear. You are then given a new space to live in by yourself with beeping noises and constant badgering. The big white lights are turned on early each morning to annoy you. As you open your eyes the people in white put more tablets down your throat before breakfast. You are now in a very regimented prison like space, everyone is now the enemy. You think to yourself “Where am I, Who are these people? When will this nightmare end?…. All this turmoil because another damn symptom arrived…….This is extreme dementia.
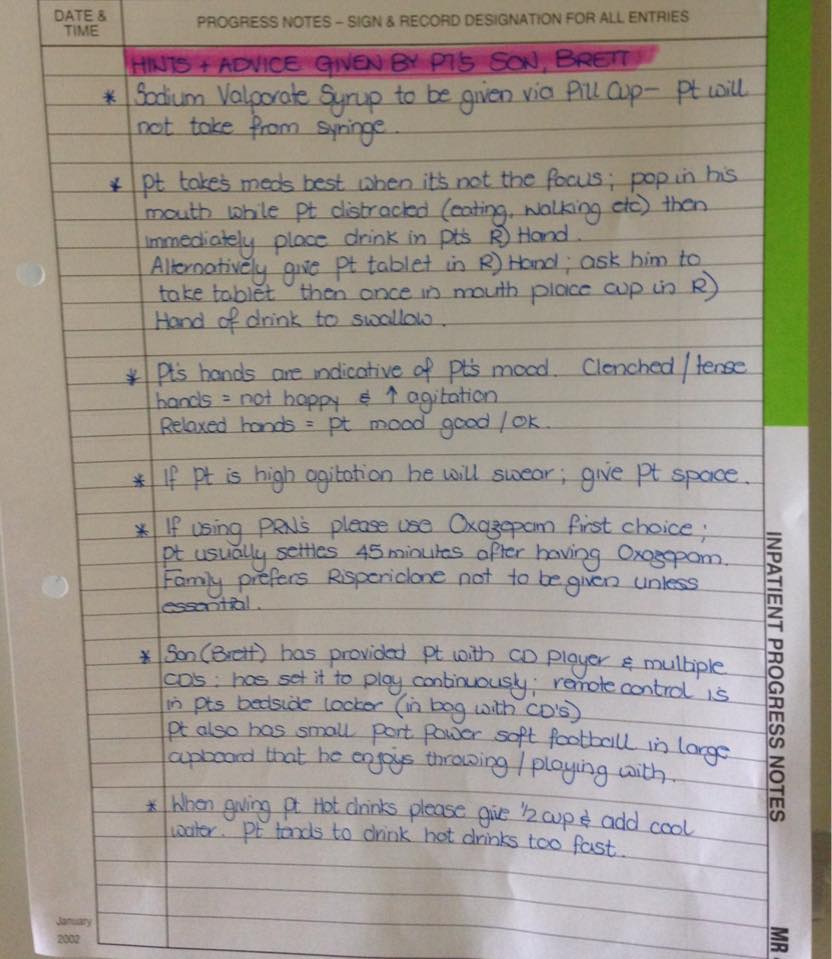
NB – The above story has been written to help us as carers ,nurses and family members possibly understand how a person with dementia feels. When you lose insight as to how ambulances and hospitals work they become very scary places indeed. We need to show empathy as much as we can and limit the distress to the person with dementia as much as possible.











 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn