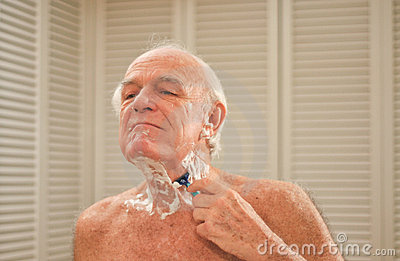
I am addressing a subject today that may not have been brought up before, but after hearing stories from family members from several different nursing homes it is a conversation that needs to be had. Shaving (and personal grooming) is a big part of caring for an elderly resident, and I would imagine the objective is to continue the routines and standards that were in place when the resident was at home.
It has been said that some nursing homes are ‘penny pinching’ by using the cheapest and nastiest razors. This is false economy in my opinion. If a ‘rough shave’ is given to a resident it will potentially cause agitation to the resident, and frustrate carers and make their role even more difficult. It will cause a painful experience for the resident, but also add more time to complete ADL’s (activities of daily living). I have even heard some carers are buying better quality razors for residents (with their own money) and storing them in their cars. I believe this is a situation that should not occur in modern times but it certainly highlights how carers feel (when they are already on low wages) yet have the decency to selflessly do this kind act for their residents. Bravo I say!
Bob uses his own electric shaver so I am not sure who bears the costs in these situations, but I assume razors are a cost that is incurred by the nursing home, unless the family wishes to provide their own? Can anybody clarify this for me?….What if the person has no family or has fallen out with their family? What are the protocols here?….I am also told that some aged care homes have towel and flannel limits per resident (eg one of each per shower). Surely in the name of hygiene and human decency extra towels can be obtained by carers if required?
We need to treat our elderly community with respect and dignity at every opportunity.












 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn