
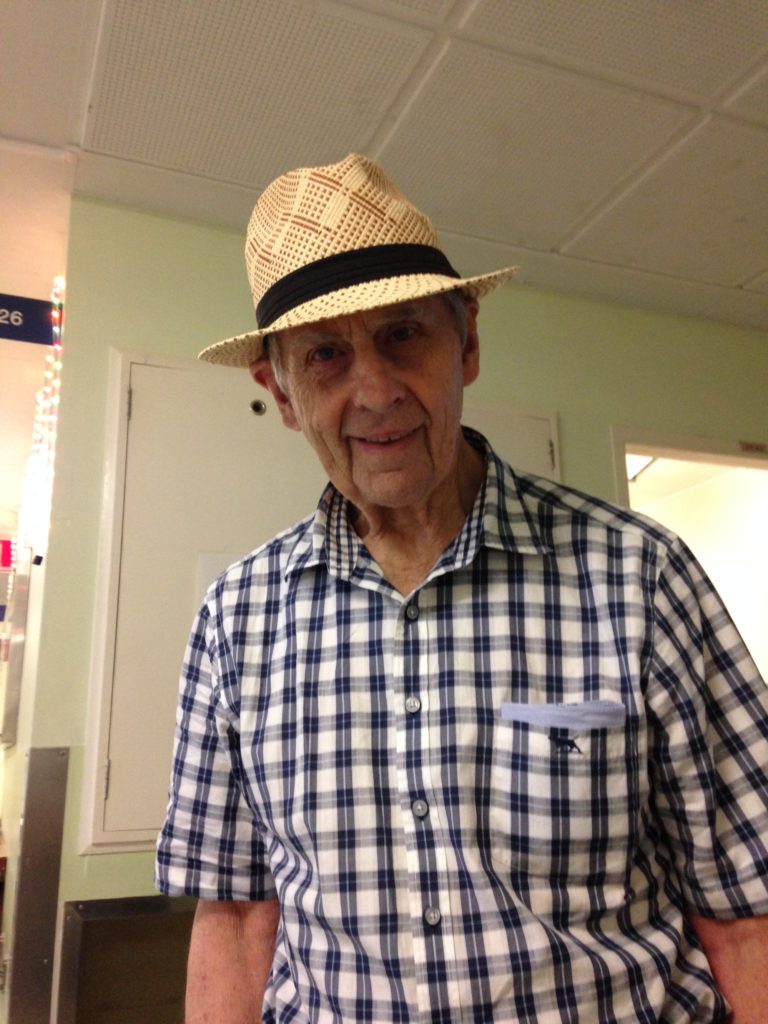
I recently went back to Bob’s nursing home to collect some items when I found myself in the middle of a hostile situation with a resident. There were two carers, a nurse and several others ‘milling around’ a resident called Barney in one of the lounge areas.Unknowingly, I walked up to Barney and shook his hand as always, and said “good morning”.
Within seconds the registered nurse (RN) pulled me away and told me to be careful as Barney was outta control and had just thrown some chairs and had tossed a glass of water over a carer to ‘cleanse him of his evil’.
The nurse also informed me that Barney had recently smashed his own television in a rage by throwing something at it. I have always had a good rapport with Barney so I asked the nurse if she was ok if I tried to calm him? She said “no problem”.
Straight away I jumped on to Barney’s side and asked him if he could show me his new room. I felt he needed to be away from others, and the change of environment may de-escalate the situation. I took him by the hand and once in his room I asked if he would mind if we sat down together for a while? He was ok with this and then I asked him how he was feeling. Barney answered “I am frustrated”. This answer was pivotal as it told me where to start digging for clues as to why he was violent. I asked him “tell me what things are frustrating you?”. Barney replied “I do not trust those people, they have messed with the chemistry and composition of the food and the drinks, and they are evil”. He said ” The Japanese cannot be trusted and the women have the codes and they can still be easily broken”. Straight away I knew he was talking about wartime and breaking secret codes.
I then tried to soothe him by playing his favourite classical music in his room. He told me it was Bach and he enjoyed it very much. I started to dig for clues as to why he was upset, and asked him some more questions. He then said to me “I only trust one person in here , but I can’t tell you who it is, we only communicate by morse code”. I was starting to think he was having some real delerium issues at this point. Barney then asked me if he could have my hand?. He held my hand and with his thumb and started to pulse and tap my palm . What I then realized was that he was typing the international morse code signal for help….SOS! (I took this as him telling me that he trusts me).
I excused myself to go and talk to the nurse to see what the medication situation was with Barney. She advised that he was refusing all meds and no-one could get near him. I knew it was unconventional, but I asked if she wanted me to try and give him his medication? The nurse said “it’s worth a try”. I then grabbed two fresh cups and his tablet and headed for Barney’s room. He was dozing in his chair listening to the music. I poured myself some water from his jug and made sure he saw me swallow it. I then poured him a drink and re-assured him that “the water is fine and is ok to drink”. (he had told me previously that the food and drink was tampered with). Because I had Barney’s trust he drank his water,and when I asked him to place the tablet in his mouth and swallow… he happily did so. I was so pleased and was silently cheering to myself.
We then sat for a few more minutes listening to his music and just talked. I advised Barney I had to leave, but thanked him for the water and the chat and shook his hand. He held my hands tightly and just kept saying to me ‘thank you, thank you for visiting me and listening to me.”
What I learnt:
- gain the trust of the resident first and then distract them
- remove them from crowded areas (eg. away from who he is arguing with)
- change the environment to a much calmer one (eg music)
- spend 5 mins or so just listening to their story, the clues may emerge.
- get into their head space, and understand how they are thinking at that very moment of time
- be creative – think outside the square when trying to find solutions
- dementia is about being flexible and changing things to suit the individual. (you cannot have a ‘one size fits all approach)
- By spending a small amount of time listening to the resident can save hours of stress and bad behaviour which can impact on the entire nursing home.














 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn