
I was walking into Ward R8 at the RAH when my mobile rang. It was the ward manager and she had bad news for me. I told her I was 5 metres from where she was calling me from , so she hung up and came and spoke to me face to face. The very caring manager explained to me that Bob had been very agitated , refused all meds and grabbed the wrist of a nurse and hurt her. An intra muscular injection was called for and I gather a security team would be on stand-by. She was concerned about me seeing the trauma of the injection being administered, but I said I have seen it done enough to be fine. I asked the manager if I could have a try at giving the meds before they inject him, and she agreed.
I walked up to Dad carefully and gave him my normal happy greeting. He had the ‘evil stare’ he gets when agitated, and I reached for his hand to feel the tension. His hand was clammy and rigid and is a tell-tale sign of his mood and aggression level. We were surrounded by 4-5 nurses who were all trying to help the situation, but actually weren’t. Straight away I put myself in dad’s shoes…how is he feeling about the situation? To him it would look like another ‘code black’ was about to happen and he would be terrified.
I held his hand with a special grip that I learnt from an expert called Teepa Snow. It is used to comfort him, make him feel in control and give me protection against a possible hit. The grip worked well, I then directed Dad away from the crowd. Straight away I went onto his side of the situation and agreed with whatever he felt or said. Once I had distracted him and calmly spoke with him, I had his trust and he was compliant. As we did a lap of the hallway – I asked the nurses to prepare meds and water for me so I can give it to him smoothly. They handed me the cup and tablets on my next walk past, and I turned dad away from the nurses. I did my usual routine, placed the tablets in the palm of his hand, gestured with my hand to place them in his mouth and then gave him the water.
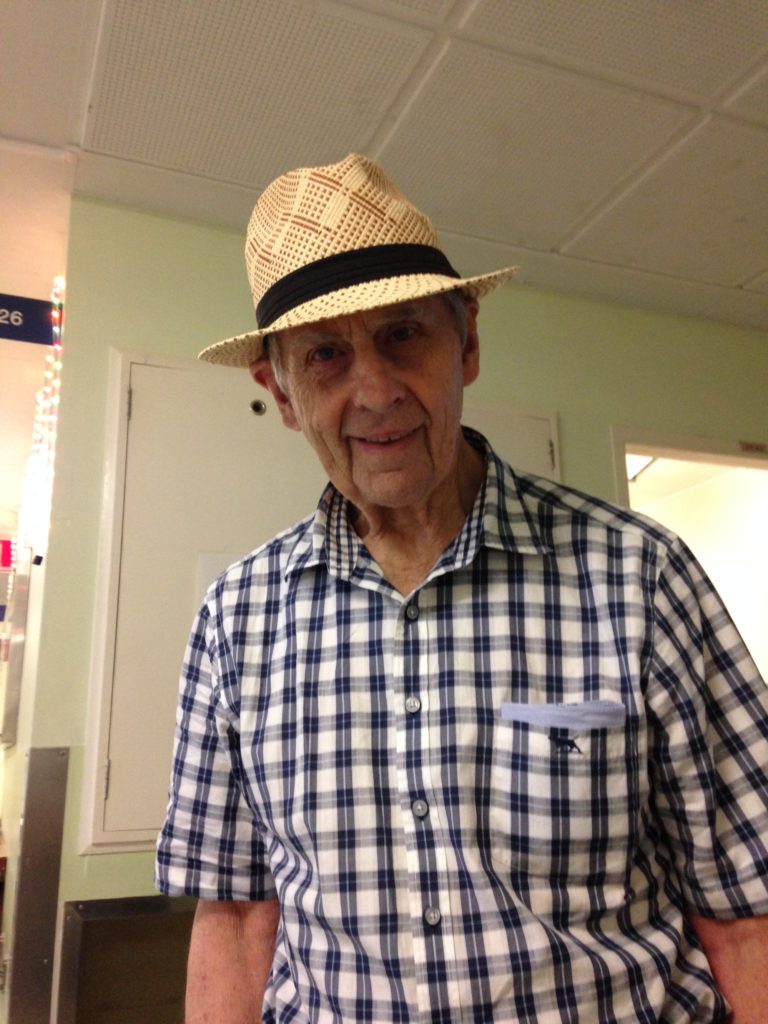
He complied instantly. The nurses were in shock as they had been trying for hours. The problem was they kept trying to give the meds to him by adding people, adding pressure and too much talk. He was confused, frustrated and also angry. I then decided to walk Dad up and down the hallways to get the medication to kick in quicker and also change the mood. More tablets were handed to me as I went past, and once again our medication routine worked a treat. After 20 minutes or so Dad’s hands loosened up, he started to smile and laugh and the incident was over. The manager ‘thanked me’ which was really nice of her.
Normally no-one would go near Dad after an agitated incident and a shower would be completely out of the question, as it is a potential hotspot. Something told me, that Dad may enjoy the water on his face if I can get him in the bathroom, and may keep him occupied. I usually start his routine by getting him to clean his teeth. If he doesn’t do it himself, I do it for him. He let me clean his teeth, so I knew we were a good chance of getting the showering done. The bathrooms in the RAH are horrendous. The shower is hand held (which means I can’t have both hands free), there are no shelves to put anything on and many people use the bathroom so they are not always clean. I asked a nurse to bring me 3 x towels and 2 x flannels asap.
You have to be extremely organised when showering, have everything on hand and be ahead of the game. I like to have a helper on the outside of the bathroom to pass me things as required.The nurse had walked off for some reason, and I was cross because I had forgotten the pull-up pants that were required. I yelled out for someone to fetch them, which they eventually did. I was starting to sweat with the steam and the tension of the moment. It is critical that I am ready with his clothes the second he is dry. I throw them on him very fast as this is another guaranteed flash point for him. Even if he can’t get his arm in his shirt sleeve within 2 seconds, he may hit out. If you don’t get his pants and shirt on fast enough he may storm out of the bathroom naked and then you have a real problem.
Amazingly I showered Dad faster than normal and had him clean and dressed within 15 minutes. The nurses were staggered with the change in his behaviour and also the fact he was showered so quickly. The reason why I was able to turn things around is I understand dementia, I know Dad’s body language back to front and also he is familiar with me. It is hard for the nurse special as most are not dementia trained and are ‘going in cold’ with no idea of what Dad is capable of and what may set him off. By simply trying to assist to take his pants off he may firmly grab your wrist or hit you. I like to let him take his own pants off always (would you like your pants pulled down for you?). If he won’t take them off I may wet his pants with the shower head and they become heavy and he then naturally removes them. You need to think outside the square with dementia.
Dad’s dressing gown cord was missing and he started to tug at the front as he felt exposed and I could tell it was annoying him. I believe he would fiddle with it all day as it kept opening, which is an unnecessary stress. I then decided if we can’t find his cord , I will make one. I asked for some scissors and made a belt from two pieces of material. I wrapped him up like a big present and he was then happy. His mood was now jovial and relaxed and everything was sorted. It was a great lesson for the nurses, to show them that dementia can be turned around without drastic measures if you know what to do. Thank goodness they rang me before calling the ‘code black’.
















 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn