I want to share something that is very personal to me, but also very public.
As many of you know, when I do a dementia presentation I leave nothing in the tank. I bare my soul and give you a ‘warts and all’ insight into a situation that is playing out all over the world many times over. I try and influence people to understand that there are millions of people battling with dementia, but there are millions more caring for these people. This is global…..
For some bizarre reason I want to share what it is like to stand in front of a group of strangers, tell my story then watch positive change happen in front of me. It is terrifying, exhilarating, emotional, therapeutic and powerful all at the same. I spend hours and hours preparing and practicing to the point of having the speech content spinning in my head out of control, and even getting upset on occasions when things hit too close to home. I have so much to say but have to find the most influential bits and try and remember them….This is the stressful part. The first 2 minutes of a presentation you are being looked at by strangers and being judged, you feel vulnerable but this goes away very soon. I choose to have a ‘this is me…and I am what I am” attitude. I try and deliver honesty and brutal reality in a sincere & authentic package and I can feel some people in the room squirm. I realise this is my speaking style and is not for everyone.
The key to public speaking is to ‘push on’ no matter what happens, as this is not about me, it is about the audience and what’s important is what they take away from the presentation. Can they be better carers and nurses with more information and real stories?…I hope so.
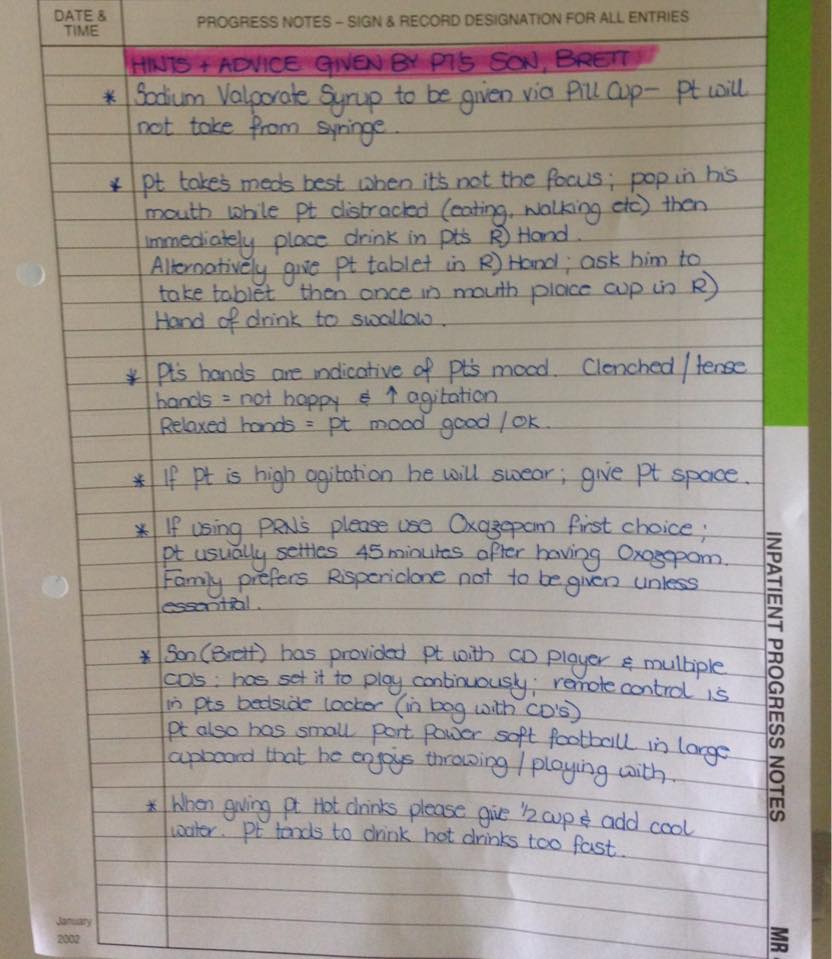
After the speech I love it when people come up and tell me their stories. This inspires me and gives me new ideas to create change. To give you an example I recently had a lady come up to me and tell me her heartbreaking story about her husband with Alzheimers who had trouble with anti-psychotics at age 57 and took his own life 3 weeks later. Another lady shared with me some amazing and unique ways to create engagement in the nursing home she works at, someone else talked about acute care issues in the country, others just say ‘thank you’. I feel so privileged to be exposed to the private lives and thoughts of others without even knowing them. I encourage these people to join ‘Dementia Downunder’ to share their thoughts and ideas with all of you. We can get to know them and deal with dementia as a community….there is strength in numbers.
I try and chip away with ‘taboo’ subjects and I brought up a new one yesterday…incontinence & toileting issues. This is happening in every aged care home, and hospital in the world and it is difficult to deal with, and our amazing carers and nurses are dealing with this many times per day. If people are struggling with an aspect of a disease we need to bring it out in the open, discuss it and then deal with it. No more restriction , no more stigma, this dementia story needs to be told ‘loud and proud’ without judgement. Let’s just have the conversation and work out the solutions. A positive and collaborative mindset is what we need without politics, excuses and old fashioned thinking….this is simply about PEOPLE, and they ALL matter irrespective of their race, gender, financial status, social problems, sexual orientation or anything else.
I leave the dementia workshop and visit my Dad which keeps me grounded as it reminds me what I am fighting for. I go back to being a son again and just sitting with him hoping for a smile. I banter with the residents and we talk about ‘nothing!’ and laugh. My sister helps me get Dad ready for bed and does a great job, as this is not easy when the person no longer knows how. I go home to my family, only to once again fall asleep on the couch exhausted with a headache from my exciting ‘rollercoaster’ day.
I want to be free when I speak and I am going to continue to ‘break the shackles’ and talk about this disease and all that comes with it. I hope I can encourage others to speak up as we need more people to share their story, we need more caring people in our aged care homes, we need to create dignity for all, the clock is ticking…..tick…tick…tick…





















 Facebook
Facebook Twitter
Twitter LinkedIn
LinkedIn